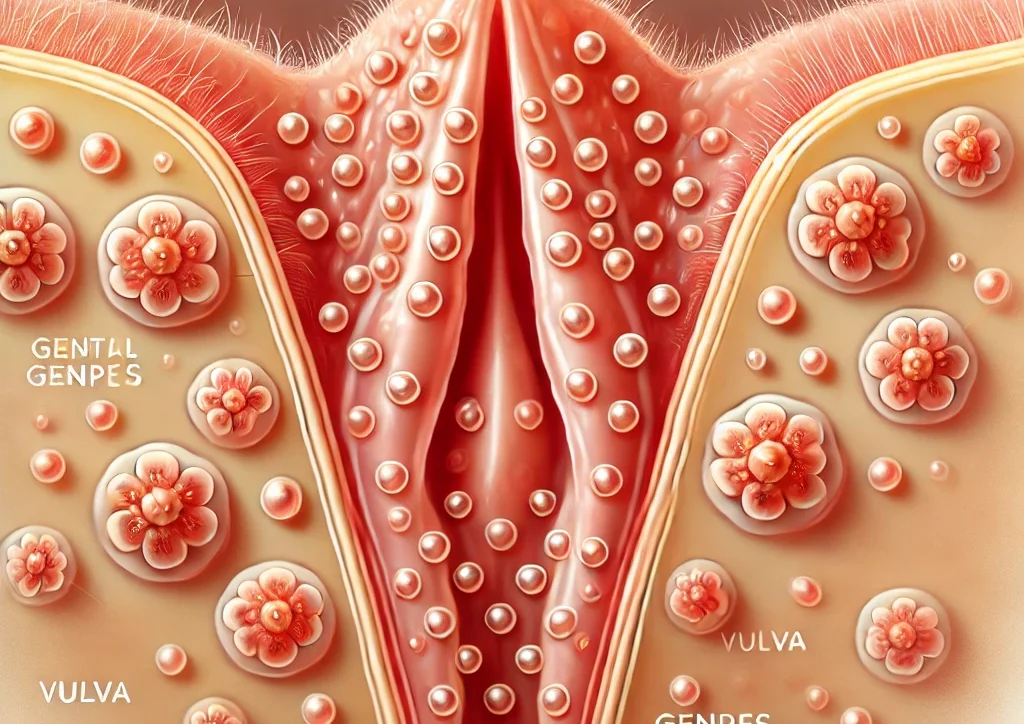
Everything You Need to Know About Genital Herpes
Genital herpes is a common sexually transmitted infection, usually caused by the herpes simplex virus (HSV-1 or HSV-2). Although it causes hardly noticeable symptoms in some people, many people do experience unpleasant symptoms. Think of itching or tingling around the genitals, pain when urinating and blisters or open wounds on the skin. These symptoms can recur in the form of so-called outbreaks, in which the virus becomes active again. The impact of this is not only physical, but can also be very heavy emotionally. How do you deal with uncertainty or fear about, for example, a new outbreak? After an infection, the virus remains inactive in the nervous system, protected from the immune system. When your immune system is weakened, for example by stress, an infection or fatigue, the virus can activate and cause an outbreak. It is therefore essential for pregnant women to avoid these triggers as much as possible. Genital herpes can in some cases pose risks during pregnancy and childbirth. A first infection during pregnancy can even cause complications. It is therefore extremely important that you are well informed and know what your specific situation requires. If you are planning to become pregnant or are already pregnant and you recognize symptoms, please contact us, we know that it can be incredibly difficult to find someone to turn to with your questions about this, but we are here for you.
Impact of Genital Herpes during Pregnancy
Genital herpes can add an extra layer of uncertainty to an already stressful pregnancy. During labor, the virus can be passed from you to your baby if there is an active outbreak and the baby can come into contact with the fluid from the blisters. Infection occurs through direct skin-to-skin contact with active herpes lesions in the birth canal. Infection can be more serious in a newborn because their immune system is not yet fully developed. Fortunately, there are precautions that we can take together to minimize this risk as much as possible. If you know you have herpes, it is important to discuss this with us as your midwives during your care during pregnancy. Regular check-ups and open communication about symptoms help us to make a good plan in time. For example, if there is an active infection around the date of delivery, a caesarean section may be necessary in the event of a first-time infection with the herpes virus to prevent transmission to the baby. If you do not tell us that you have blisters around your vagina for the first time and that it may be your first herpes infection, this is dangerous for the baby's health. A caesarean section may sound drastic, but together we will ensure that you and your baby receive the best care. If you have had a herpes infection before, it is a different story. Because the infection can flare up again when your immune system is reduced, it may sometimes be advisable to consider preventive antiviral medication during the last weeks of your pregnancy. These medications can reduce the risk of an outbreak around the time of delivery. We will discuss this with you in detail so that you have insight into all the options. We believe that correct information and guidance are crucial during this period and we know that you need this as a pregnant woman if you are familiar with the herpes virus.
Emotional impact and support
Getting pregnant is exciting, but how do you prepare for something you’ve never experienced before? Getting genital herpes can be emotionally draining, both before, during, and after pregnancy. However, during pregnancy, a herpes outbreak can be even more emotional, and you may feel overwhelmed by concerns about your health and that of your baby. You may be wondering, How do I talk to my partner about this? Keep in mind that every expectant parent has uncertainties—you’re not alone. Genital herpes can bring up feelings of guilt, shame, or isolation. The question of how you got the infection or the idea that you may have passed it on can be especially hard on your mind. For pregnant women, this can be compounded by the fear of transmission during childbirth. These uncertainties are understandable, but knowing that there are safe ways to protect your baby can be a great comfort. It’s important to talk about this, both with your partner and your midwife. Open communication with your partner and midwife is crucial. Explain what you’re feeling and what you need. Perhaps you are looking for emotional support or just want someone to listen without judgement. Together you can plan how to best deal with the situation, which will help to relieve the pressure. Midwives like us at PuurBegin offer comprehensive care and guidance. Don’t hesitate to share your fears and questions during consultations. Other things that can help is focusing on relaxation to reduce the chance of an outbreak by having as little stress as possible. Think of mindfulness or a calm breathing technique that brings back your focus, but yoga can also be very effective. Remember that low-threshold support, such as a listening ear from a family member, can also make a difference. With us, your well-being is not just about your physical health. Whether it is about mental support, relationship questions or practical advice, we will look together at how we can best support you during this special time.
How do you get genital herpes?
Genital herpes is usually transmitted through sexual contact with an infected partner, even if the partner does not show visible symptoms. The virus can still spread during a time without symptoms.
How is genital herpes diagnosed?
The diagnosis of genital herpes is usually made by a health care provider who will evaluate your symptoms, perform a physical exam, and possibly take a sample of the blisters or sores for laboratory testing. Furthermore, a herpes infection can occur in two forms: herpes type 1 and 2. To determine which type of herpes virus you have, a culture of the fluid from the blisters can be taken. However, taking these cultures is painful and there is no added value in doing this during pregnancy.
How is a genital herpes attack provoked?
Factors that can trigger an outbreak include stress, illness, fatigue, hormonal changes or even UV light. Everyone can react differently and that is why it is good to keep track of what your triggers are. During your pregnancy it is important to try to get your vitamins by eating enough fruit (2 pieces per day) and vegetables but also to get enough rest. Especially if you are familiar with the herpes virus, fatigue is something to listen to carefully. If you have had a bad night, try to get some rest the next day.
How do I prevent genital herpes?
To reduce the risk of transmission, it is advised to:
- Use latex or polyurethane condoms.
- Do not have sex during an outbreak.
- Open and honest communication with your partner about your condition.
How common is genital herpes?
Genital herpes is a common condition worldwide. Studies estimate that approximately 1 in 6 adults between the ages of 14 and 49 have the herpes virus. However, because it is rarely talked about, you often do not realize that there is a good chance that you know someone who knows how you feel.
Herpes and the desire to have children
If you are planning to become pregnant and have genital herpes, don't be discouraged. Many women with this condition have healthy pregnancies and babies. It is important to talk to your obstetrician about your herpes history, especially if you have or have had an active outbreak in the past.
Vaginal birth is still possible
Pregnant women with a 'dormant' genital herpes infection can simply give birth vaginally. Even if you have had genital herpes before and are now having a new outbreak, you can simply give birth vaginally. This is because there is a minimal chance of infection to the baby, because the blisters around your vagina are taped off or smeared with iodine tincture. Only if you have never had genital herpes before and are now having a very first infection in the last 6 weeks until delivery or during delivery itself, a caesarean section is chosen because there is a risk of transmitting the virus to the baby if you were to give birth vaginally.
Hospital protocols
Hospitals have specific protocols when a woman with genital herpes is in labor. However, if you have had a genital herpes infection before, there is no medical indication for labor and you can simply give birth with your own midwife. However, it may sometimes be the case that a hospital has made arrangements with the midwife for check-ups of the baby after birth to prevent possible infections to detect, for example a one-off check by the pediatrician to be on the safe side.
Important points for the conversation with your midwife
At your first appointment with your obstetrician, it is crucial to share your history of genital herpes. Discuss:
- The frequency and severity of your outbreaks.
- Your concerns about the birth and the health of your baby.
What if my baby is infected after birth?
As discussed earlier, there is no objection to a vaginal birth if you have ever had a herpes infection. The risk of infection is present if you have had a herpes infection for the first time and also have an active first outbreak during labor. If a baby contracts genital herpes during labor, this can lead to serious health problems, including infections of the skin, eyes or brain. However, it is good to know that the serious consequences of an infection do not occur very often: 2 to 3 children per 100,000 births.
Treatment and Prevention
Treatment for genital herpes focuses primarily on managing symptoms and preventing further outbreaks, as there is no cure. Antiviral drugs, such as Aciclovir, can reduce the duration and severity of outbreaks. But did you know that your daily choices can also affect the course of the condition? A healthy lifestyle often helps manage stress, a major trigger for herpes outbreaks. Regular relaxation, a balanced diet and adequate sleep can all make a big difference. Diet also plays a crucial role. Try to avoid foods that contain arginine, such as nuts and chocolate, as these can activate the herpes virus.
Treatment usually includes antiviral drugs such as aciclovir and often a zinc oxide ointment is also prescribed to relieve symptoms. If you regularly suffer from recurring outbreaks, it is possible to start a maintenance course of oral aciclovir. This is done in consultation with your GP, who may refer you to a gynaecologist for a proper assessment of whether a maintenance dose is necessary. Furthermore, antiviral drugs such as aciclovir and valaciclovir are safe and effective during pregnancy. They can help to relieve symptoms and minimise the chance of transmission to the baby.
You cannot cure genital herpes
It is important to realize that genital herpes is a chronic condition. While there are treatments that can relieve symptoms and reduce outbreaks, there is currently no cure for genital herpes.
Learning to live with genital herpes
Learning to live with genital herpes can be challenging, but many people with the condition live full and healthy lives. Education, communication with partners, and good self-care are essential to maintaining a positive life with herpes.
Midwifery Support PuurBegin
Genital herpes can not only cause physical discomfort, but also be emotionally taxing, especially during pregnancy. Understanding your body and the signals it gives helps you get a grip on the situation. With us, care is not just about treatment, but also about guidance. How do you feel about this? Do you need emotional support? We are here for that. Being pregnant can make you vulnerable and herpes outbreaks can feel extra confusing or worrying during this period. In addition to medical guidance, your emotional and practical needs play a major role. Together we discuss how you feel stronger and safer. For example, think about planning consultations in which we take all the time to answer questions. This offers a space in which you feel taken seriously.
Conclusion
Genital herpes is a chronic condition that can impact pregnancy and pregnancy. It is important to be well-informed and actively collaborate with healthcare professionals. Open communication with your obstetrician can help ensure a safe and healthy pregnancy experience. Remember that there are effective treatments and support available to help you manage genital herpes, so you can focus on building a future with your baby.
Stay informed!
Follow us on social media for the latest news and a look behind the scenes Midwives PuurBegin in Kampen. Discover the daily adventures of our midwives, valuable tips for expectant parents and inspiring stories from the field. Click on the buttons below and stay connected with our heartwarming team!
 |
 |
Take care of yourself and your little one!
With kind regards,
Address: Orkestlaan 148, 8265RC Kampen
Telephone: 085 40 19 095